Re-credentialing is challenging for Payors, and it's costlier than what it appears to be keeping track of Payor re-creds, sending applications, follow-ups, and handling incomplete applications.
Significant percentage of providers get dropped out of the Network during re-creds as the application never reached the right person at the right time.
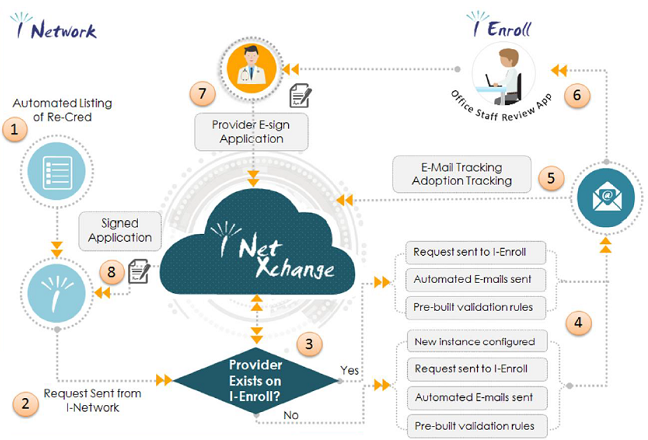
I-Network's Provider Directory Solution automates the process of notifications and follow-ups. With an intuitive and easy to use online web portal and e-Sign capability, the solution enables you to send out Directory Verification and update request electronically and allow providers to update and attest the information from anywhere, anytime.